 Alzheimer’s disease (AD) could be the next frontier for deep brain stimulation (DBS) therapy.
Alzheimer’s disease (AD) could be the next frontier for deep brain stimulation (DBS) therapy.
A small phase 1 pilot study showed that some patients with AD who received constant stimulation to the fornix — the principle outflow tract from the hippocampus — had increased hippocampal volume after 1 year.
There was also some evidence that this increased hippocampal volume correlated with cognitive benefit.
These results, published online in Brain Stimulation, suggest that fornix stimulation affects the structure of the brain and, if replicated, would be promising for AD treatment.
“In Alzheimer’s disease, the brain, in particular the hippocampus, melts away; as you lose your hippocampus, you lose your memory, and so far, there is nothing that can stop or slow down this process,” said study author Andres Lozano, MD, a neurosurgeon at Toronto Western Hospital and professor and chair, neurosurgery, University of Toronto, Ontario, Canada.
“If we are able to apply electrical stimulation, and if indeed we’re able in some cases to slow down or even reverse the process, it would be a very exciting finding.”
A second, larger study, a double-blind, randomized trial in 42 patients, is about to wrap up and should soon shed more light on the effectiveness of DBS in AD, the researchers say.
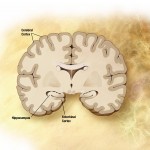
Circuit of Papez
Characterized by atrophy in the hippocampus as well as other brain structures, AD involves amyloid and tau deposition, formation of neurofibrillary tangles, and cerebral hypometabolism, the authors note. These processes result in dysfunction in several neural circuits, including the memory circuit of Papez.
DBS has already been proven effective for movement disorders, such as Parkinson’s disease, tremor, and dystonia. It’s also being used experimentally to treat patients with intractable psychiatric conditions, including major depression, obsessive-compulsive disorder, and anorexia nervosa.
Although the mechanism of action is uncertain, experts believe it likely involves modulated activity within dysfunctional neural circuits. But the prevailing thought has been that DBS is unable to influence progressive neurodegenerative processes acting on these circuits.
The current study included six patients with AD who participated in a phase 1 clinical trial showing that the DBS procedure was safe and could alter brain metabolism. These patients with AD were the first in the world to receive DBS, according to Dr Lozano.
The patients — four men and two women — were relatively young (aged 51, 69, 58, 62, 60, and 64 years) and had received the diagnosis of probable AD within the previous 2 years. They had a spectrum of dementia from mild to moderate and severe.
After electrodes were implanted, these patients received constant mild stimulation of the fornix. From structural MRI scans, researchers measured the volume of the hippocampus, fornix, and mammillary bodies — critical components of the Papez circuit — at baseline and after 1 year of continuous stimulation. They also looked for evidence of brain-wide structural changes.
At the end of the study period, two of the six patients (patients 1 and 4) showed a striking increase in right and left hippocampal volume. The mean (average of right and left) hippocampal enlargement was 5.6% in patient 1 and 8.2% in patient 4.
Caught by Surprise
“Not only did the hippocampus not shrink in these patients but the thing that caught us completely by surprise was that it actually grew and it grew by a large amount,” said Dr Lozano.
He noted that the baseline Alzheimer’s Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) score for these two patients (18.67 for patient 1 and 11.67 for patient 4) indicated relatively mild AD.
Hippocampal volume did not increase in the other four patients, but their baseline ADAS-Cog scores were higher. “They were too far along and the circuit too destroyed or damaged that there was no one home to stimulate,” commented Dr Lozano.
“We think there may be a point of no return where damage is so extensive that you can’t recuperate function. Our feeling is that the earlier you go in, the more likely there will be something to rescue and something to work with.”
The researchers compared these hippocampal volume changes to a control group of 25 persons matched for age, sex, and neurocognitive severity who did not receive DBS. MRI data at baseline and at 12 months for these controls were available from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database.
No hippocampal growth occurred in any of these 25 controls. “So we think this does not occur spontaneously in Alzheimer’s disease, that it has occurred as a consequence of the brain stimulation in this case,” commented Dr Lozano.
Circuit Training
He believes that the stimulation is reactivating the memory circuit that is atrophying in AD. “It’s almost like circuit training, putting the circuit on a treadmill and making it work, and in so doing so, we think that the circuit can be maintained.”
Studies show that rodents receiving DBS actually generate more neurons, he added. “If this were to occur in humans, maybe we would have a way of repairing these damaged circuits. That’s important because you would go from a purely symptomatic treatment to actually treating the root cause and modifying the course of the illness.”
The hippocampal volume increases in the two patients appeared to correspond to cognitive outcome. Patient 4’s ADAS-Cog score improved from 11.67 at baseline to 7.33 at 1 year. Patient 1 did not have an improved ADAS-Cog score but showed the least deterioration among the other patients.
“Those whose hippocampus grew either got better cognitive function or stabilized whereas in those where it shrunk, cognitive function continued to deteriorate as expected in a progressive disease like Alzheimer’s disease,” said Dr Lozano.
The study also found evidence that fornix stimulation was associated with clusters of local volume expansion in temporoparietal regions of the brain that, although far from the Papez circuit, are known to be atrophic in AD.
The study did not find enlargement of the fornix or mammillary bodies. However, patients 1 and 4 showed the slowest atrophy rate in both of these structures, possibly suggesting a circuit-wide structural effect of fornix DBS.
Patient 4, who opted to continue to receive DBS, was reimaged at 3 years. After the 4-point improvement at year 1, this male patient got worse again (ADAS-Cog score of 15.33). But Dr Lozano pointed out that the average per year drop in this score in patients with AD is 7 points.
“So we would expect him to go from 11 to 18 to 25. That’s not what happened; he went from 11 to 7 to 15. We think that is possibly significant; it’s different than the expected natural course.”
Glucose Metabolism
Researchers also measured hippocampal glucose metabolism using positron emission tomography (PET) with a radio tracer. They did this preoperatively and in the “on” stimulation condition following 12 months of continuous DBS.
They found increased glucose metabolism — indicating the brain is using fuel — but it’s not clear how this is connected to increased hippocampal volume, said Dr Lozano. “We think the two are linked, but we don’t know which one comes first or whether one leads to the other or they’re independent.”
According to Dr Lozano, noninvasive stimulation methods, such as transcranial magnetic stimulation, would not produce the same results. For one thing, DBS provides targeted and precise stimulation “24/7,” which wouldn’t be possible with other modalities. In addition, the fornix is located at the center of the brain, which would be difficult to reach externally.
Would a stronger stimulus produce even better results? Possibly, he said, but when researchers at one point turned up the stimulation to a very high level, it produced unwanted vivid memories in some patients. The current settings were arrived at through patient input.
Information on the two patients whose hippocampus got bigger and whose illness stabilized has informed the next year-long study. The multicenter, randomized, blinded study included only patients with milder AD. Half of the 42 enrolled patients received DBS and the other half a sham treatment (electrodes were implanted but not turned on).
Cutting Edge
Medscape Medical News invited Howard Chertkow, MD, professor, neurology, McGill University, and director, aging and Alzheimer’s research axis, Lady Davis Institute, Jewish General Hospital, Montreal, Quebec, Canada, as well as scientific director, Canadian Consortium on Neurodegeneration in Aging, to comment on this new study.
Dr Chertkow applauded Dr Lozano, whom he called a “very respected” world expert in neuromodulation in DBS. The new research, he said, is “cutting edge” and the study findings “certainly novel.”
Because there are limited effective treatments for AD, which affects almost 36 million people worldwide, and its cause is not yet confirmed, “any new treatment, any new lead, certainly has to be pursued,” he said.
The suggestion that stimulating the memory network can improve memory and is accompanied by changes on MRI and PET “is very exciting” and indicates that the results “are not just serendipitous,” added Dr Chertkow.
Another encouraging aspect of the study for Dr Chertkow is that it provides “the first clear evidence in humans” that stimulation might produce neurogenesis. “If we can create new connections in the hippocampus, maybe we can do so in a whole range of other brain disease, even beyond Alzheimer’s disease.”
But Dr Chertkow pointed out what he sees as negative aspects of the DBS approach used in the study. For example, the stimulation targets memory and so the best result is improved memory, but AD also involves changes in personality, emotions, and other cognitive functions, such as planning and language.
“There are other brain networks involved and it doesn’t seem logical that if you impact on one network that you are going to necessarily improve things in other networks.”
AD is a degenerative disease characterized by deposition of toxic proteins, such as amyloid and tau. “It’s doubtful that this treatment is going to stall or attenuate or stop this process,” said Dr Chertkow. “While it might improve symptoms, it’s not really attacking the disease itself.”
Other disadvantages to DBS in AD are that it’s invasive and costly and so “will always have limited applicability,” said Dr Chertkow.
“This is not going to be the answer for Alzheimer’s disease and memory loss with aging around the world, but it may have a role.”
Dr Lozano received support from the Surgeon Scientist Program, Department of Surgery, University of Toronto, and Neurosurgical Research and Education Foundation of the American Association of Neurological Surgeons. He is a Canada Research Chair in Neuroscience and is supported by the R.R. Tasker Chair in Functional Neurosurgery. Additional support was provided by the Dana Foundation and Krembil Neuroscience Discovery Fund. Dr Lozano is a consultant to Medtronic, St. Jude, and Boston Scientific; serves on the scientific advisory board of Ceregene, Codman, Neurophage, Aleva, and Alcyone Life Sciences; is cofounder of Functional Neuromodulation Inc; and holds intellectual property in the field of deep brain stimulation. Dr Chertkow has disclosed no relevant financial relationships.
Brain Stim. Published online December 3, 2014.